Nirupama Putcha, Gabriel G. Paul, Antoine Azar, Robert A. Wise, Wanda K. O’Neal, Mark T. Dransfield, Prescott G. Woodruff, Jeffrey L. Curtis, Alejandro P. Comellas, M. Bradley Drummond, Allison A. Lambert, Laura M. Paulin, Ashraf Fawzy, Richard E. Kanner, Robert Paine, III, MeiLan K. Han, Fernando J. Martinez, Russell P. Bowler, R. Graham Barr, Nadia N. Hansel, for the SPIROMICS investigators
Chronic obstructive pulmonary disease (COPD) is a leading cause of death, not just in the US but also worldwide. Patients with COPD are at increased risk for various respiratory infections, which are main contributors to COPD exacerbations. Selective IgA deficiency is associated with higher risk of respiratory infections, however, a link between serum IgA levels and COPD disease activity has never been established. The goal of this study is to test the hypothesis that sub serum IgA levels is associated with increased morbidity in COPD patients, using participants from the SPIROMICS cohort. Serum was collected at enrollment, and IgA levels were measured using the Myriad RBM biomarker discovery platform. Deficient IgA was defined as <7mg/dL and subnormal level defined as ≤70mg/dL. Follow-up was conducted yearly at the clinic and quarterly by phone for up to 3 years.
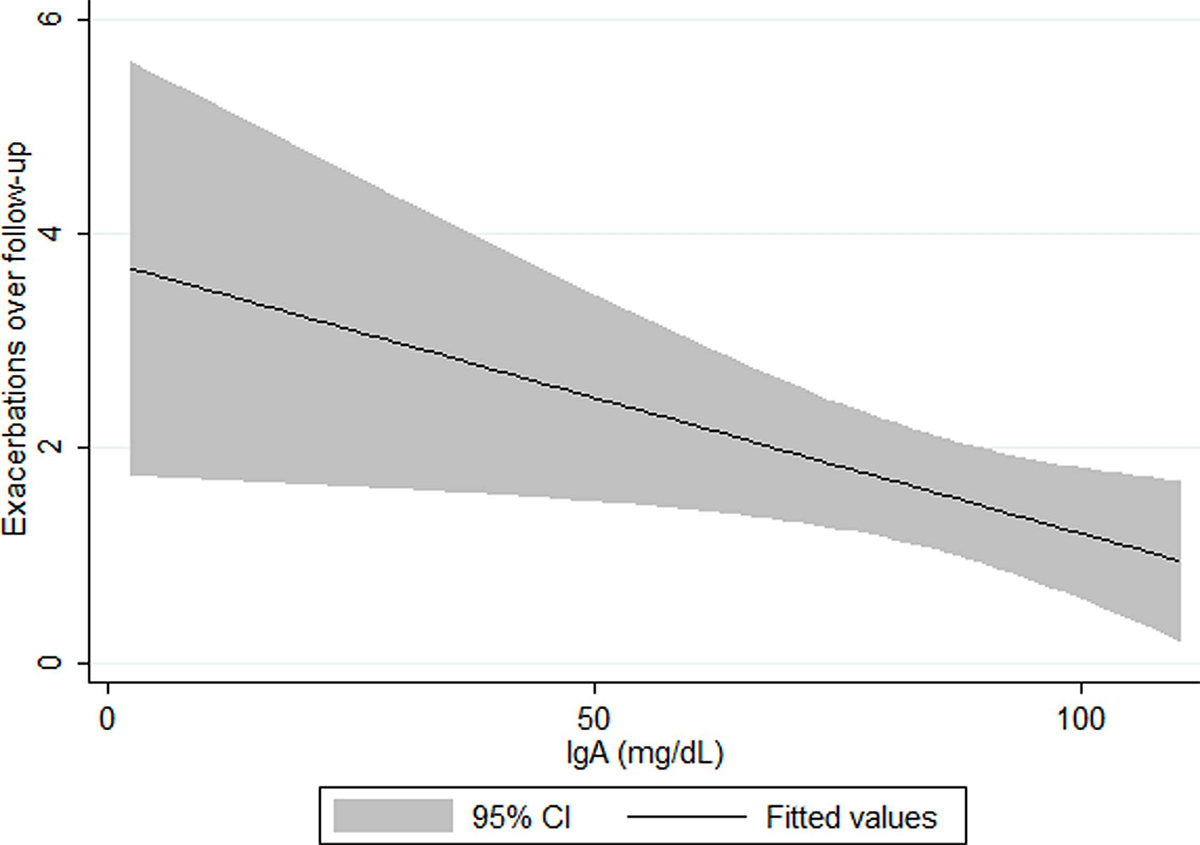
At enrollment, the mean IgA level (269.1 mg/dL) was comparable to the general population. Only 1 subject had deficient IgA and 25 participants had subnormal IgA levels. Participants with subnormal serum IgA have increased exacerbations compared to those with normal serum IgA during follow-up. Additionally, participants with IgA levels <120mg/dL demonstrated a dose-response, with higher number of exacerbations with decreasing serum IgA.
This study demonstrated a novel correlation between serum IgA levels and increased risk of COPD exacerbations, indicating a possibility that COPD patients with subnormal IgA are more susceptible to infections.